Folks who suffer from hemochromatosis, or know someone who does, often wonder whether plant-based diets offer any unique benefits to those with iron-overload.
The significance (if any) of the vegan diet in the etiology, prevention and treatment of hemochromatosis is unknown as there are no studies directly investigating the effects of 100% whole food plant-based diets on the management of this condition.
That’s not to say there is no relationship. According to L. Kathleen Manahan and Janice L Raymond, authors of Krause’s Food and the Nutrition Care Process, “individuals with iron overload should ingest less heme iron from meat, fish, and poultry compared with nonheme iron from plant foods.”1
So at least in regards to this specific imperative, it could be beneficial to follow a diet excluding animal products, deriving dietary iron exclusively from plant sources.
Further, according to James Barton author of Hemochromatosis: Genetics, Pathophysiology, Diagnosis, and Treatment, “hemochromatosis is rarely seen in vegetarian populations, and about two-thirds of body iron in meat eaters is derived from absorption of heme iron.”2
While the relationship of the vegan diet with hemochromatosis (often an entirely genetic condition) is far from elucidated–due to very little research–there’s definitely some relationship between iron status and dietary choices.
If you want to know more, then read on. I’ll cover what the condition is, and then go over the role of diet in iron status, and how the vegan diet specifically may offer some benefits.
What is Iron Overload?
Iron, a component of our red blood cells, and an extremely important mineral in many bodily processes is acquired through the diet and other environmental sources–from pollutants to the cast-iron skillets we cook in.
Of the iron we ingest, we:
- Use it of course, as mentioned
- Store the excess for later. This excess iron is stored in macrophages of the liver, bone marrow, and spleen.
- Excrete the rest via daily “obligatory loss”–a small amount (about 1mg) of iron is lost daily through the skin, gastrointestinal tract, and urinary tract.3-6
Because the capacity for excretion is quite limited (1mg), and storage space is finite as well, the main mechanism by which our body regulates iron levels is by absorption–how much our body allows the absorption of iron contained in a given food.
Iron overload comes about by excessive iron intake in one form or another:
- The accidental incorporation of iron into the diet via environmental sources–the most common way. In developing countries, it’s often due to the consumption of foods cooked in cast iron cookware, or foods grown in contaminated soils.
- The over-ingestion of iron. In developed countries, iron overload is often the result of excessive iron-supplementation, iron-fortified foods, etc.
The Effects of Iron Overload
While iron is an essential nutrient absolutely crucial for many bodily processes, it causes a lot of damage in high amounts:
- It loves to exchange electrons, creating free radicals that damage DNA, and cellular structures. Because oxidative damage is implicated in nearly every chronic disease, this one feature incriminates iron overload in a host of conditions.
- Excessive iron in the body has been linked to a number of diseases and conditions. Everything from heart disease, type 2 diabetes, and Alzheimer’s disease*, to hypertension, cancer, and fatty liver disease.
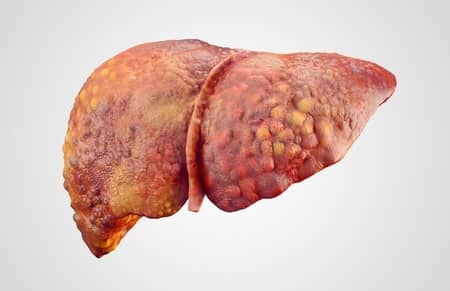
Cirrhotic liver with fatty degeneration
*As brain iron increases with age, and is elevated in neurodegenerative diseases, such as Alzheimer’s disease and Parkinson’s disease.7
A few of the uncommon disorders associated with iron overload include:
- Alcoholic cirrhosis–the most advanced form of liver disease
- Chronic hemolytic anemia–a form of anemia due to hemolysis, which is the abnormal breakdown of RBCs
- Porphyria anemia–a group of disorders resulting from the buildup of certain chemicals related to RBC proteins.
- Aplastic anemia–
a “ normochromic-normocytic” anemia, a rare condition wherein the body stops producing enough blood cells.
Hemochromatosis
Hemochromatosis is the most common form of iron overload. It eventually leads to progressive organ damage–hepatic, cardiac, pancreatic, etc.
It’s particularly damaging because people with this condition absorb up to THREE TIMES more iron from their food than those without the condition. It’s particularly pernicious, as it often goes undiagnosed.
Men are more susceptible to damage from hemochromatosis than women, as they have no physiologic mechanisms for losing excess iron (menstruation, etc.).8
Because of the hyper-absorption, it’s easy to see how diet plays an important role in the outcomes. Someone could be consuming loads of iron in the form of red meat, multi-mineral supplementation, etc. all the while with unregulated absorption of the iron.
What’s the Relationship Between the Vegan Diet and Hemochromatosis?
Well, as mentioned in the opening of the article, hemochromatosis is rarely seen in vegetarian populations, and most body iron in meat eaters is obtained from the absorption of heme iron.
So, in
As I’ll touch on, heme iron is the type of iron that the body has no mechanism by which to regulate its absorption.

So, even those without a genetic condition impeding the absorption of nonheme iron are still powerless to regulate the absorption of heme iron.
Dietary iron exists in one of two forms:
- Heme iron–the type of iron that’s primarily derived from hemoglobin and myoglobin. For this reason, it is found naturally in meat, poultry, and fish. Now, these animal products still contain nonheme iron, but about 50%-60% of the iron in these foods sources is in the form of heme iron. Various supplements and fortified food products also contain this form of iron.9
- Nonheme iron–the type of iron found primarily in plant foods–fruits, vegetables, nuts, grains, and tofu. Dairy products also contain a bit of nonheme iron, but overall dairy represents a very poor source of iron in general. Unless fortified, these food sources don’t contain any heme iron.9
While non-heme iron absorption is regulated by how much iron you currently have stored in your body, heme iron gets a free pass.
The exclusive consumption of nonheme iron poses some risks in terms of achieving adequate iron status, but provides protection against insidious iron overload, because when iron stores are full, the body simply downregulates absorption. This is great in that chronically high levels of iron are implicated in many diseases.
However, with genetic hemochromatosis, there’s a pathology of this protective mechanism. All of a sudden the body can’t regulate iron from nonheme sources, and it becomes nigh impossible to achieve iron homeostasis.
So, if hemochromatosis negates one’s ability to regulate the absorption of heme iron, how is it that vegetarian populations have lower incidences of the condition?
The answer is that no one knows for sure. However, keep in mind that both heme and nonheme iron are contained in meat, fish, and poultry. Folks who eliminate these sources of iron are mostly only consuming the latter–which have much less total iron content.
After all, vegetarians and vegans especially are constantly told to ensure they’re getting sufficient iron–and rightfully so.
Therefore it stands to reason that this population would be less likely to accumulate iron in the blood, all else equal. After all, heme or nonheme, plant foods–unfortified–have less iron overall compared to sources such as meat, fish, and poultry.
References
It should also be noted that there are many plant foods that enhance or impede iron absorption, but that’s an article for another time.
- Krause’s Food & the Nutrition Care Process L. Mahan-Janice Raymond – Elsevier – 2017
- Hemochromatosis: Genetics, Pathophysiology, Diagnosis, and Treatment James Barton-Corwin Edwards – Cambridge University Press – 2000
- Dubach R, Moore CV, Callender S. Studies in iron transportation and metabolism. IX. The excretion of iron as measured by the isotope technique. J Lab Clin Med 1955;45:599–615.
- Green R, Charlton R, Seftel H et al. Body iron excretion in man. Am J Med 1968;45:336–53.
- Weintraub LR, Dennis DJ, Conrad ME et al. Iron excretion by the skin. Selective localization of iron59 in epithelial cells. Am J Pathol 1965;46:121–7.
- Cole SK, Thomson AM, Bellewicz WZ. Hematologic characteristics and menstrual blood loss. J Obstet Gyn Br Common 1972;79:994–1001.
- Bartzokis G, et al: Prevalent iron metabolism gene variants associated with increased brain ferritin iron in healthy older men, J Alzheimers Dis 20:333, 2010.
- Moretti D, et al. Relevance of dietary iron intake and bioavailability in the management of HFE hemochromatosis: a systematic review, Am J Clin Nutr 98:468, 2013.
- Gropper, Sareen S.; Smith, Jack L.. Advanced Nutrition and Human Metabolism (Page 482).