One common question I get from people considering making the switch to a vegan diet is whether or not a whole-food plant-based eating pattern will be any match for very high levels of cholesterol with largely a genetic basis— i.e. what’s known as familial hypercholesterolemia.
So, I thought I would take the time to write the following article outlining the science of the vegan diet in the context of hypercholesterolemia.
It seems promising, but currently, no one knows with any certainty whether or not the vegan diet offers unique benefits when it comes to improving the lipid profiles of those with familial hypercholesterolemia.
I stress the word familial because while there are numerous studies looking at the effects of 100% plant-based diets on lipid profiles, there are no studies directly investigating the relationship between the vegan diet and hereditary hyperlipidemia.
Anyway, having said the above, there is no reason to doubt that a 100% plant-based diet wouldn’t help manage blood lipids in this population insofar as it helps lower LDL and total cholesterol in general.
I personally have a history of high cholesterol and lost nearly 80 points on my cholesterol when switching to a 100% plant-based diet, and I really believe you can do the same (see my blood work at the bottom of the article).
The real question of interest is something like this: are the positive effects of the vegan diet on hypercholesterolemia sufficient so as to offset/compensate for the increased risk of heart disease incurred by having the genetic condition.
The answer to that question is likely yes. After all, many of the mechanisms by which a plant-based diet is thought to lower cholesterol are independent of the role that the liver plays in putting out too much cholesterol (e.g. increased excretion of cholesterol, etc.).
According to a meta-analysis published in Annals of Internal Medicine, a dietary emphasis on the inclusion of nutrient-dense plant-based foods decreases levels of low-density lipoprotein cholesterol (LDL-C) in adults with hypercholesterolemia.1And it did so more than the already effective eating patterns recommended by national guidelines.
If you’re a nutrition nerd like me and want to know the nuts and bolts of just how the vegan diet might be in a unique place to help those with genetic hyperlipidemia, then read on.
This is an area that is near and dear to my heart, as I have this genetic propensity for extraordinarily high cholesterol levels as does my mother. For this reason, I cover the subject here with a fine-toothed comb and even post my own blood work.
Just What is Familial Hypercholesterolemia?
To begin, we better cover a few other “-emias”
Hyperlipidemia
Because “lipid” is the broadest term for the organic compounds that are oily or waxy to the touch (think fatty-acids, cholesterol), genetic hyperlipidemia is the umbrella term for conditions resulting in increased serum lipids.
So hyperlipidemia could be hypertriglyceridemia or any number of hypercholesterolemias.
Similarly, there is a “dyslipidemia” which is defined as a blood lipid profile that increases the risk of atherosclerosis development. It’s used for classifying the following dyslipidemias.
Familial Hypercholesterolemia (FH)
Or type IIa dyslipidemia is what’s known as a monogenetic disorder, and involves defective genes for the LDL receptor. In this variant, elevated cholesterol is present from birth, and for this reason, results in early atherosclerotic disease.
Remember, atherosclerosis (fatty plaque buildup in the arteries) takes YEARS to develop in most people. It usually takes decades of an unhealthy diet to result in enough fatty deposition to occlude arteries.
However, those with FH have a running start on everyone else. From a young age, they have lipids floating around at levels most don’t achieve until adulthood. This one is screened for by performing an ultrasound of the Achilles tendon for the presence of what’s known as xanthomas (cholesterol deposits from LDL-C).
Polygenic Familial Hypercholesterolemia
This one results from multiple gene defects, with one on what’s known as the apo E-4 allele being common–not important for these purposes. Those with polygenic FH tend to have lower LDL-C levels, however, are still at high risk of premature disease.
Screening, in this case, involves having one’s familial history checked: two or more family members with an LDL-C in the > 90th percentile is typically the criteria.
Familial Combined Hyperlipidemia
In this version, there are defects in various genes leading to the overproduction of apo B-100 and hepatic lipase (LPL). Just know that it results in an enzyme not being able to do its job in moving fat around–i.e., it can’t effectively remove triglycerides (TGs) from the bloodstream.
Thus, the TGs build up and tend to hang out causing all kinds of trouble. This one is screened by patients having 2 or more family members with an LDL-C or TG in the > 90th percentile. There is one more type, known as familial dysbetalipoproteinemia, but it’s fairly uncommon so we won’t go into it here.
How Could The Vegan Diet Be Uniquely Beneficial?
Inquiry into the potential role of plant-based dietary protocols in controlling lipid levels of adults with hyperlipidemia began with a bit of simple deduction
- It’s well established that elevated levels of LDL-C put one at higher risk for cardiovascular diseases
Dietary modification has long been considered the first approach in the treatment and control of CVD.2,3
However, initial efforts to modify diet to achieve desired outcomes focused on avoiding deleterious food components such as saturated fat and dietary cholesterol.4-6 Results from such efforts showed these interventions to be effective, but modest.7
Unlike diets traditionally used in studies of this nature, the vegan diet shines in two respects: by virtue of what it excludes (harmful animal products) and by what a well planned, whole-food, plant-based vegan diet includes–ample amounts of dietary fiber, vitamins, nutrients, antioxidants, and phytochemicals.
In recent times, researchers have begun to take a second look at the oversimplified focus on avoiding certain dietary components and started to look to what may need to be included in an effective dietary strategy in the prevention of heart disease.
It just so happens that beneficial dietary components thought to improve many cardiovascular parameters are entirely of plant origin. Gee, what a coincidence.
The plant kingdom includes a vast range of food groups and constituents established as beneficial to one’s lipid profile: 7-13
- Soy proteins
- Soy isoflavones
- Soluble fiber
- Oats
- Garlic
- Plant sterols
- Nuts
Real World Results
The article referenced above followed individuals for four weeks noting changes in cholesterol levels between a Low-Fat and Low-Fat Plus. The Plus group received copious amounts of healthy, whole-plant foods to complement the dietary fat and cholesterol restriction. Results were as follows1:
- Total Cholesterol (TC): -0.24 mmol/L (-9.2 mg/dL) versus -0.46 mmol/L (-17.6 mg/dL) (P = 0.01)
- LDL Cholesterol: -0.18 mmol/L (-7.0 mg/dL) versus -0.36 mmol/L (-13.8 mg/dL) (P = 0.02)
Between-group differences:
- Total-C: -0.22 mmol/L (-9 mg/dL) (95% CI, -0.05 to -0.39 mmol/L [-2 to -15 mg/dL])
- LDL-C: -0.18 mmol/L (-7 mg/dL) (CI, -0.04 to -0.32 mmol/L [-2 to -12 mg/dL])
Neither group differed significantly in high-density lipoprotein cholesterol (HDL), and triglyceride levels.
My Bloodwork
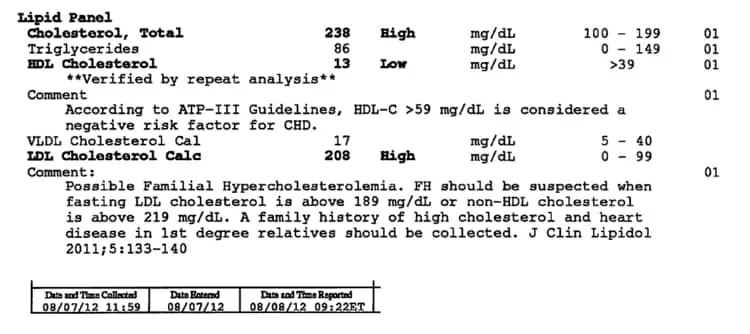
I had my bloodwork taken a few times over the course of several months, and the results were quite shocking.
It’s long been suspected that I have familial hypercholesterolemia. My mother is the same way—she eats very little saturated fat and still struggles with high cholesterol levels.
As you’ll see in the attached picture, my previous numbers were horrific! I had scores of 238, 13, and 208 mg/dL for total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), and LDL-C, respectively.
As you can see from the reference values, any one of these numbers alone would put anyone at
Luckily I was able to nip this problem in the bud by my late 20’s (upon starting the vegan diet), but obviously earlier would’ve been better.
As I’ve covered in various other articles, even if you’ve accumulated substantial plaque (what they call foam cells and fatty streaks), the vegan diet can still help reverse the condition, as it’s the only diet to show efficacy in removing plaque and reversing heart disease.
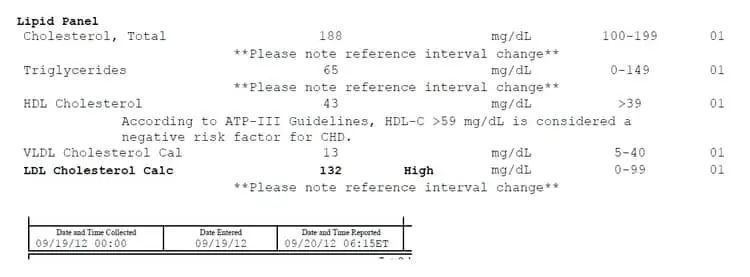
This is from a couple of months after. Great improvement, but not quite there.
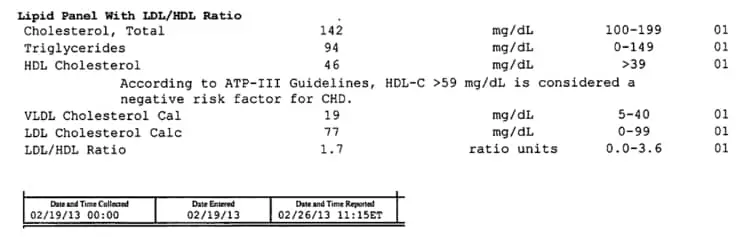
And finally, most recent numbers have approached the coveted heart attack free zone, though there is still some room for improvement—I would definitely like to see higher HDL numbers. Overall, I’m very excited about the results.
Anyway, if you or a loved one suffers from familial hypercholesterolemia, adopting a whole food, plant-based diet may be just what’s needed to mitigate, or potentially reverse the damage done by chronic, high levels of cholesterol.
If it is a loved one, please send them this article so they can see for themselves the potential effects of following a whole food plant-based diet.
Conclusion
In closing, I would say that you should always consult your physician on measures you should take to treat or prevent a health condition. It’s long been thought that a healthy diet can help manage FH–after all, dietary recommendations are part of the lifestyle therapy that doctors prescribe alongside drugs like statins.14
But, according to the Mayo Clinic (among other sources), diet therapy is only one component of the overall approach to managing FH, along with increasing physical activity levels, maintaining a healthy body weight, and you guessed it… drug therapy. 15
This comes as bad news to many, because a lot of people seek out specialized diets in hopes that they can be used to replace invasive treatments or drugs that are thought to be unnatural or unhealthy.
While diet therapy can help with the management and prevention of certain diseases, the remedy of many conditions–especially those with a largely genetic basis–is beyond the scope of what can be accomplished with any lifestyle modifications.
References
- Gardner CD, Coulston A, Chatterjee L et al. The effect of a plant-based diet on plasma lipids in hypercholesterolemic adults—a randomized trial. Ann Intern Med. 2005;142:725–733.
- Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143-421.
- Krauss RM, Eckel RH, Howard B, Appel LJ, Daniels SR, Deckelbaum RJ, et al. AHA Dietary Guidelines: revision 2000: A statement for healthcare professionals from the Nutrition Committee of the American Heart Association. Circulation. 2000;102:2284-99.
- Summary of the second report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel H). JAMA. 1993;269:3015-23.
- Chait A, Brunzell JD, Denke MA, Eisenberg D, Ernst ND, Franklin FA Jr, et al. Rationale of the diet-heart statement of the American Heart Association. Report of the Nutrition Committee. Circulation. 1993;88:3008-29.
- Krauss RM, Deckelbaum RJ, Ernst N, Fisher E, Howard BV, Knopp RH, et al. Dietary guidelines for healthy American adults. A statement for health professionals from the Nutrition Committee, American Heart Association. Circulation. 1996;94:1795-800.
- Anderson JW, Johnstone BM, Cook-Newell ME. Meta-analysis of the effects of soy protein intake on serum lipids. N Engl J Med. 1995;333:276-82.
- Crouse JR 3rd, Morgan T, Terry JG, Ellis J, Vitolins M, Burke GL. A randomized trial comparing the effect of casein with that of soy protein containing varying amounts of isoflavones on plasma concentrations of lipids and lipoproteins. Arch Intern Med. 1999;159:2070-6.
- Law M. Plant sterol and stanol margarines and health. BMJ. 2000;320:861-4.
- Kris-Etherton PM, Krummel D, Russell ME, Dreon D, Mackey S, Borchers J, et al. The effect of diet on plasma lipids, lipoproteins, and coronary heart disease. J Am Diet Assoc. 1988;88:1373-400.
- Ripsin CM, Keenan JM, Jacobs DR Jr, Elmer PJ, Welch RR, Van Horn L, et al. Oat products and lipid lowering. A meta-analysis. JAMA. 1992;267:3317-25.
- Sabate J, Haddad E, Tanzman JS, Jambazian P, Rajaram S. Serum lipid response to the graduated enrichment of a Step I diet with almonds: a randomized feeding trial. Am J Clin Nutr. 2003;77:1379-84.
- Ackermann RT, Mulrow CD, Ramirez G, Gardner CD, Morbidoni L, Lawrence VA. Garlic shows promise for improving some cardiovascular risk factors. Arch Intern Med. 2001;161:813-24.
- Cameron T Lambert, et al. Current Treatment of Familial Hypercholesterolaemia. Eur Cardiol. 2014 Dec; 9(2): 76–81.
- Familial Hypercholesterolemia. https://www.mayoclinic.org/diseases-conditions/familial-hypercholesterolemia/diagnosis-treatment/drc-20353757