Inflammation is a necessary part of healing and is used by the body to fight illness and disease. Ironically, the very process designed by evolution to protect the body can lead to disease in the long term.
This is likely because inflammation, while initiated for tissue repair and adaptation, may involve collateral damage. This is particularly relevant to obesity and its associated metabolic dysfunctions, such as CVD, type 2 diabetes, and cancer.
Such conditions lead to chronic systemic low-grade inflammation which promotes numerous pathologic and self-propagating events, including dysfunction of the endothelium, insulin resistance, and activation of cancer pathways.1
One of the best measures one can take prevent inflammation is to adopt an anti-inflammatory diet. An anti-inflammatory diet involves eating specific anti-inflammatory foods while avoiding offending foods in order to minimize levels of inflammation in the body.
With a few tweaks, the anti-inflammatory diet as laid out by numerous health organizations maps on almost perfectly to whole food plant-based diets. Obviously, the quality of such diets can vary quite widely depending on how they’re employed. But, if you follow the guidelines in this article, you can rest assured that your vegan dietary practices will be as anti-inflammatory as possible.
A quick note: this article provides general guidelines. The absolute best resource on using specific vegan foods in the right quantities to lower inflammation and prevent chronic diseases can be found here.
What Is an Anti-Inflammatory Diet?
The anti-inflammatory diet is a diet proven to be useful for the treatment of inflammatory diseases, most notably rheumatoid arthritis (RA). It’s thought that it works by reducing the expression of genes that are involved in inflammatory processes such as those responsible for TNF-a and IL-1, IL-6.2
As laid out for non-vegans, it resembles the Mediterranean diet as it emphasizes including as much fresh food as possible while eliminating processed food and added sugar. It encourages the consumption of vegetables and fruit (especially berries), nuts, legumes, dietary fiber and EFAs (omega 3s).
Sound familiar? It sounds a lot like a vegan whole food plant-based diet. The main difference is that it encourages lean protein by suggesting sources like fish and chicken.
How Does the Standard Anti-Inflammatory Diet Compare to the Plant-Based Variant?
Well, the standard anti-inflammatory diet suggests sourcing lean protein from animals. However, that’s not to say that lean protein is superior from such sources. The experts who designed this diet assumed (and rightly so) that most people want to consume some types of meat in their diet. If you read my article on protein, you know that the plant kingdom offers numerous sources of high-quality lean protein.
It should be noted that fish is recommended in the traditional anti-inflammatory diet due to its high omega 3 as well as protein content. However, many plant foods (especially flaxseed) offer ample amounts of omega 3s. As for DHA and EPA, these can be acquired through various certified vegan supplements.
So, all in all, a well-planned vegan diet stacks up quite well against the standard anti-inflammatory diet and may even be superior in some respects—which we’ll get into later.
What Are Anti-Inflammatory Foods?
Anti-inflammatory is not just a trendy health food term. Foods deemed as anti-inflammatory meet criteria set forth by the Dietary Inflammatory Index (DII)—a system that’s been developed and validated to serve as a tool to assess the overall inflammatory potential of a given diet. The criteria are based on over 6,500 peer-reviewed research papers and are made up of 45 nutrients, bioactive compounds, foods, and spices.
The foods and compounds were studied in relation to six inflammatory markers:3,4
- Interleukin 1b (IL-1b)
- Interleukin 4 (IL-4)
- Interleukin 6 (IL-6)
- Interleukin 10 (IL-10)
- Tumor necrosis factor alpha (TNF-a)
- C-reactive protein (CRP)
Finally, each food and component was rated with an Overall Inflammatory Effect Score with negative numbers given to food components having the most anti-inflammatory effect. You don’t need to know any of this because the below recommendations are based on this model taking all the guesswork out.
The 9 Pillars of an Anti-Inflammatory Vegan Diet
Below are the main components of an anti-inflammatory diet adapted to plant-based diets. Fresh foods and avoidance of overly processed food items are stressed in this dietary pattern, and as you’ll see, fresh whole food is really the common denominator.
1) Include a Wide Variety of Fruits and Vegetables—Every Color (9 Servings Minimum)
Colorful fruits and veggies contain the whole gamut of anti-inflammatory dietary components that are thought to provide the bulk of the benefits seen with this diet for reducing inflammation in the body.
This is based on the fact that fiber and bioactive compounds contained in this food group have been shown to down-regulate inflammatory biomarkers such as histamine, Nuclear Factor-kappa Beta (NFkB), C-reactive protein (CRP), and numerous cytokines both in vitro and in vivo.5-8
Most plant-based foods contain decent anti-inflammatory properties, especially compared to animal products, but the following fruits and veggies are listed because they’ve been demonstrated to be the most anti-inflammatory and are mentioned the most often in research:9-11,8
- Onions, and fresh garlic
- Cruciferous vegetables
- Purple grapes
- Berries
- Cherries
- Citrus fruits
- Pomegranates
- Tomatoes
2) Add Herbs and Spices to Your Meals

Anti-inflammatory herbs and spices include:5,9-11
- Black and green tea
- Turmeric (perhaps the most anti-inflammatory)
- Ginger
- Rosemary
- Oregano
- Fenugreek
- Caraway
- Anise
- Cocoa
- Mint
- Clove
- Coriander
- Cinnamon
- Nutmeg
- Red chili powder
- Lemongrass
- Fennel
- Saffron
- Black pepper
- Parsley
- Sage
- Dill
- Bay leaf
- Basil
3) Eat The Right Kinds of Fats (20-30% of Your Daily Calorie Intake)
Include Foods High in Omega 3 EFAs and Monounsaturated Fats (MUFAs)–2 Tbsp./Day Minimum
Sources of unsaturated fats that are high in omega-3 fatty acids (alpha-linolenic acid) are known to be anti-inflammatory.
The best plant-based sources of omega-3 include:
- Flaxseed
- Chia seed
- Hemp seeds
- Walnuts
A note on oils—yes, some plant oils (namely, walnut and flaxseed) do contain relatively high omega 3 content. However, the fatty acids in oil tend to get oxidized easily, so it’s best to stick with whole food. Not to mention, oils have a mere fraction of the phytonutrients and antioxidants present in the plants they were derived from.
Consume Lots of Monounsaturated fats (MUFAs)
Omega’s 7 and 9 are the most common MUFAs in the human diet. Evidence continues to indicate that of the beneficial effects MUFA consumption provides, the fatty acid is especially good at reducing risk of CVD and other diseases where inflammation is implicated.12
The Mediterranean diet became famous for its anti-inflammatory effects. The diet was known for including high amounts of olives and olive oil which contain high amounts of omega 9. For the reasons specified, I’d recommend sticking to whole food. Avocados (omega 7) and olives are two of the best MUFA sources.
Limit Saturated Fatty Acids and Foods Rich in Omega-6 Fatty Acids
Don’t get me wrong, omega-6 FAs (linoleic acid) are considered essential fatty acids for a reason. But, the molecule is pro-inflammatory especially when eaten in high amounts relative to omega 3s—which is easy to do.
Further, while omega-6 from whole foods can be problematic if you’re not consuming sufficient omega-3 FAs, processed foods—namely oils and oil-rich junk food—are often the culprit when excessive omega 6 consumption is a problem.
So, limit oils especially the kind that’s really high in linoleic acid:
- Soybean oil
- Corn oil (a huge offender!)
- Safflower and sunflower oils
Eliminate Hydrogenated Fats
Partially hydrogenated fats (trans fats) used to be ubiquitous in processed and prepackaged foods. Lawmakers really started to crack down a few years ago and it’s at the point now where you may not even encounter the stuff. In the US, trans fats were banned for use in processed foods back in July of 2015 and were completely removed from shelves 3 years later.
The consumption of trans fats has been shown to increase levels of inflammation and has been strongly linked to coronary artery disease.13
Fully hydrogenated oils are still around—you’ll usually find them in vegetable shortenings (Crisco) and margarine. And while perhaps not quite as deleterious as trans fats, they’re at least as bad as saturated fats, so you’ll want to avoid them.
4) Consume Nuts Daily (1/4 Cup Minimum)
Nuts contain not only EFAs but are also rich in micronutrients and phytochemicals many of which have been shown to lower inflammatory markers.
Nuts contain vitamin E, folic acid, copper, magnesium, potassium, and even dietary fiber.
Substances that are commonly found in nuts include:14
- Phytoestrogens—isoflavones and lignans
- Flavonoids
- Phenolic acids
- Transresveratrol
- Phytosterols
- Tannins
- Phytates
- Tocotrienols and tocopherols α-tocopherol.
As mentioned, EFAs (especially their ratios in the diet) are important when it comes to controlling inflammation. Nuts and seeds provide the aforementioned anti-inflammatory compounds, and many provide omega-6 and omega-3 FAs in ratios that have been shown to support a beneficial inflammatory response.15
You’ll want to consume a wide variety of nuts in order to get the full spectrum of the nutrients listed above. Nuts that have been shown to be especially beneficial are:
- Almonds
- Brazil nuts
- Cashews
- Brazil nuts
- Walnuts
5) Eat a Low Glycemic Diet

It appears that excessive intake of sugars and other refined carbohydrates may be pro-inflammatory. Getting your carbohydrates in this form is problematic for two reasons:
- First, regular consumption of high glycemic foods increases blood glucose and insulin levels. Chronically elevated glucose and insulin trigger an inflammatory response in the body.
- Secondly, consuming sugar and refined carbs displaces healthier low glycemic foods which have been shown to reduce postprandial (a fancy term for post-meal) glucose and insulin levels.16 What’s more, healthy complex carbohydrates have been shown to result in lower concentrations of insulin-like growth factor (IGF-1) and lower levels of inflammatory biomarkers such as adipocytokines which are inflammatory proteins that are secreted by your fat cells.16,17
Glycemic Load vs Glycemic Index
There are tons of charts you can reference to check the effect various foods have on blood glucose levels. It turns out that glycemic load is a better metric than glycemic index, as the former takes into account food portions. For example, beets (a very healthy food) have a high glycemic index (64), but a low glycemic load (5).
Glycemic Load of Select Foods
Below is a sample list of the glycemic load of various plant foods. Sticking to whole food will largely take care of this, but the chart should give you an idea of the glycemic load of processed vs refined foods.
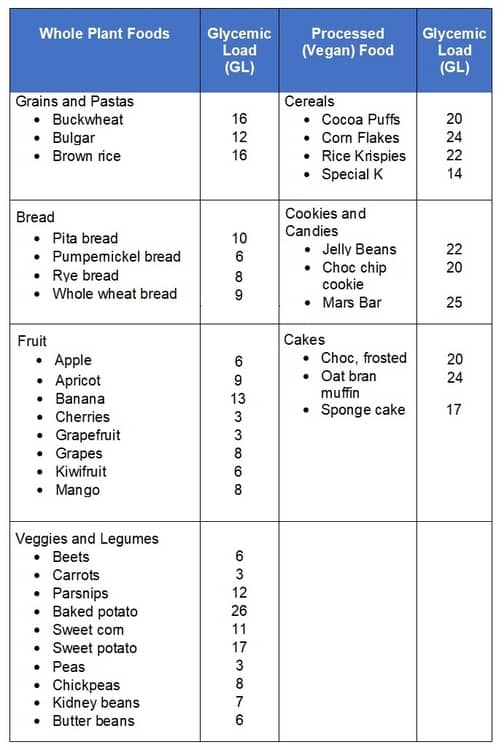
Source: Adapted from Krause’s Food & the Nutrition Care Process (Page 1053). L. Mahan-Janice Raymond – Elsevier – 2017
What This Means In Practice
Limit Refined Carbohydrates
Think white bread, pasta, white rice, table sugar and sugar-containing products like cookies, pastries, cakes, candy and energy bars. This goes for supposedly healthy granola-type bars that are high in added sugars.
Consume Lots of Whole Grains
Include lots of whole grains in your diet like bulgur wheat, brown rice, quinoa, amaranth, and spelt.
6) Consume Lots of Lean Plant Protein (10-35% of Your Daily Calories)
This is one area where vegan diets may provide an edge over standard anti-inflammatory diets. Animal protein contains a lot of the pro-inflammatory EFA arachidonic acid, which has been shown to increase inflammation when consumed in excess. The omni version of the diet encourages chicken and fish over red meats for this reason. But, plant-based protein beats out the leanest of animal-based protein in this regard.
7) Consume Lots of Phytonutrients
We talked about the importance of eating plenty of fruits and vegetables when it comes to lowering inflammation in the body. But let’s face it, not all plant foods are created equal. Plants like iceberg lettuce and cucumber contain mostly water (compared to other plant foods) and thus contain little in the way of antioxidants, micronutrients, and phytochemicals.
Foods known to have lots of bioactive compounds include:18
- Dark red fruits like berries
- Bright red and yellow fruits and veggies like tomatoes, red and orange peppers, etc.
- Dark leafy greens of course
- Cruciferous veggies like broccoli, cabbage, brussels sprouts, and cauliflower
- Soy foods—these are high in phytoestrogens.
- Tea—especially green, white, and oolong
- Cacao (nibs, powder, etc. – not candy!)
8) Consume Plenty of Plant-Based Pre- and Probiotics
It’s become increasingly evident over time that there’s an intimate relationship between gut ecology and immune function. So, it’s thought that the microbiome likely plays a significant role in reducing inflammation in the body. When most people think of probiotics, dairy yogurt comes to mind. However, the plant kingdom offers many healthy vegan-friendly probiotic sources
Fermented and cultured vegan foods that are known to provide excellent sources of probiotic bacteria include:
- Miso, a fermented soy product. If you read the article on vitamin K, you know that miso is also a rare source of plant-based vitamin K2.
- Soy yogurt
- Tempeh
- Kombucha (a fermented tea)
Sauerkraut and kimchi also contain probiotics but are high in salt.
Eating sufficient whole grain products and legumes, as discussed previously, will ensure you get adequate amounts of prebiotics in your diet. Prebiotics don’t contain the bacteria, but instead, provide your healthy gut bacteria with the fuel it needs to populate.
Specific prebiotics that are known to fuel good bacteria include:
- Inulin and fructooligosaccharides—these are found in asparagus, bananas, onions, garlic, artichoke, and chicory.
- Resistant starch found widely in grains and legumes.
- Fermentable and semi-fermentable fibers (hemicellulose, etc.) found abundantly in fruit and legumes
9) Consider Food Allergies and Food Sensitivity Elimination
While the food recommendations made thus far are considered healthy to most people, food tolerance can vary drastically between individuals. For example, while whole grains have been shown to confer many positive health effects, folks with celiac disease incur a net negative health effect by eating gluten-containing foods.
As discussed in the article on bloating, a food allergy is a food that triggers a systemic immune-mediated response involving both the innate (mast cells, macrophages) system and the adaptive immune system (e.g. antibodies).
In contrast, a food sensitivity or intolerance occurs within the gut and is often the result of an enzyme deficiency or a reaction to chemicals in the food—either a food additive or a naturally occurring chemical.
Food sensitivities and intolerances induce what is known as adverse reactions to food (ARFs). These reactions trigger the production of numerous inflammatory mediators including:19
- Cytokines
- Immunoglobulins
- Histamine
Intensity and onset of the reactions vary and depend on the dose consumed and individual tolerance. Risk of having these reactions is thought to depend on one’s exposure to food early in life, GI microflora balance, and diet quality.
You’ve probably heard of the big 8 allergens, but I’ll list them here. These are the allergens deemed common enough to list on food labels.
- Milk, eggs, and fish which we needn’t worry about thankfully
- Wheat
- Tree nuts
- Peanuts
- Shellfish (some vegans choose to eat bivalves due to their having a very rudimentary nervous system).
Common food intolerances include:
- Gluten
- Lactose
- Soy
- Histamine
- Salicylate
Finally, there are food additives that give some people issues. These are not considered as severe as the above but can be problematic for some people. These include:20
- Sulfites
- Tartrazine (Yellow 5)
- Benzoic acid
- Monosodium glutamate (MSG)
- Solanine*
If you think you may have an intolerance, the standard protocol is to eliminate the suspect foods and additives for a period of at least two weeks while assessing symptoms to see if they improve.
*Potentially. The literature is a bit weak on this one in terms of causing inflammation. Solanine is compound common to the nightshade family of fruits and veggies.
Other Measures to Reduce Inflammation
Exercise and Maintain a Healthy BMI
Weight should be maintained within the healthy BMI range. Overweight status, especially obesity, is the common denominator in terms of the comorbidities of the various chronic diseases plaguing the Western world. Excessive fat leads to insulin resistance, and as we saw previously, fat cells store inflammatory molecules known as adipocytokines.
“Adipokines” is a term used to refer a number of bioactive proteins secreted by adipocytes (fat cells). They include leptin, adiponectin, IL-6, and TNF-alpha. Anyway, the latter two (IL-6 and TNF-a) are adipocytokines. The more fat you have the more potential storage of these inflammation-inducing molecules.
Avoid Harmful Chemicals
Many of the chemicals and pesticides commonly used in the agricultural industry can disrupt the immune system causing inflammation. To reduce exposure to these chemicals, opt for organic foods and “green” cleaning and personal care products.
BPA Caution
A lot of healthy foods such as legumes come in cans. A lot of canned foods contain the compound bisphenol A (BPA) in the can linings. BPA is an endocrine (hormone) disruptor and impairs insulin action in the body, which triggers inflammatory pathways.21
The molecule can also be found in many plastic bottles and containers (food containers, etc.). Choose dry beans and look for the “BPA-Free” cans when purchasing canned goods. It may be a good idea to use glass bottles and containers when possible.
Reduce Stress and Get Adequate Sleep
Both chronic stress and lack of adequate sleep have been implicated in the etiology of inflammation.
Sleep deprivation and stress lead to an elevation in circulating cortisol which is associated with high levels of inflammatory cytokines. Long-term “sleep debt” has been shown to elevate the inflammatory biomarkers, IL -1b, IL-2, IL-4, TNF- a and MCP-1 (monocyte chemoattractant protein-1).22
A lot of studies have shown meditation to be useful in managing stress as the practice has been demonstrated to reduce the inflammatory response in experimental models.23
So, that is the WFPB version of the anti-inflammatory diet. Hope you learned a lot and hope to see you in the next article.
References
- Baffy G, Loscalzo J: Complexity and network dynamics in physiological adaptation: an integrated view, Physiol Behav 131:49, 2014.
- Krause’s Food & the Nutrition Care Process (Page 796). L. Mahan-Janice Raymond – Elsevier – 2017
- Shivappa N, et al: Designing and developing a literature derived population based dietary inflammatory index, Public Health Nutrition, 17(8): 1689–1696, 2013.
- Garcia-Arellano A, et al: Dietary Inflammatory Index and Incidence of Cardiovascular Disease in the PREDIMED Study, Nutrients 7(6): 4124–4138, 2015.
- Jungbauer A, Medjakovic S: Anti-inflammatory properties of culinary herbs and spices that ameliorate the effects of metabolic syndrome, Maturitas 71:227–239, 2012.
- Habauzit V, Morand C: Evidence for a protective effect of polyphenolscontaining foods on cardiovascular health: an update for clinicians, Ther Adv Chronic Dis 3(2):87–106, 2012.
- Hagenlocher Y, Lorentz A: Immunomodulation of mast cell nutrients, Mollecular Immunol 63:25–31, 2015.
- Jiang Y, et al: Cruciferous vegetable intake is inversely correlated with circulating levels of proinflammatory markers in women, J Acad Nutr Diet 114(5):700-8.e2, 2014.
- Aggarwal B, Shishodia S: Suppression of Nuclear Factor Kappa-B Activation Pathway by Spice-Derived Phytochemicals, Ann NY Acad Sci 1030: 434–441, 2004.
- Habauzit V, Morand C: Evidence for a protective effect of polyphenols-containing foods on cardiovascular health: an update for clinicians, Ther Adv Chronic Dis 3(2):87–106, 2012.
- Galland L: Diet and Inflammation, Nutr Clin Prac 25:634–640, 2010.
- Douglas G Mashek and Chaodong Wu. MUFAs. Adv Nutr. 2015 May; 6(3): 276–277.
- Bendsen NT, et al: Effect of industrially produced trans fat on markers of systemic inflammation: evidence from a randomized trial in women, J Lipid Res 52(10):1821-1828, 2011.
- Joan Sabaté-Rosemary; Ratzin-Turner. (2001). Vegetarian Nutrition. Page 351. CRC Press. ISBN 0-8493-8508-3.
- Sears B, et al: Anti-Inflammatory Nutrition as a Pharmacological Approach to Treat Obesity, Journal of Obesity 2011. pii: 431985. Doi:10.1155/2011/ 431985.
- Runchey SS, Pollak MN, Valsta LM, et al: Glycemic load effect on fasting and post-prandial serum glucose, insulin, IGF-1 and IGFBP-3 in a randomized, controlled feeding study, Eur J Clin Nutr 66(10):1146–1152, 2012.
- Neuhouser ML, Schwarz Y, Wang C, et al: A low-glycemic load diet reduces serum C-reactive protein and modestly increases adiponectin in overweight and obese adults, J Nutr 142(2):369–374, Feb 2012.
- Reference: Arthritis Foundation: Anti-inflammatory diet, 2014. Accessed August 2015 from: http://www.arthritis.org/living-witharthritis/ arthritis-diet/anti-inflammatory/anti-inflammatory-diet.php Boeing H et al: Critical review: vegetables and fruits in the prevention of chronic diseases, Eur J Nutr 51:637, 2012.
- Krause’s Food & the Nutrition Care Process (Page 1041). L. Mahan-Janice Raymond – Elsevier – 2017
- Wilson B, Bahna S: Adverse reactions to food additives, Annals of Allergy, Asthma & Immunology 95(6):499–507, 2005
- Valentino R, et al: Bisphenol-A Impairs Insulin Action and Up-Regulates Inflammatory Pathways in Human Subcutaneous Adipocytes and 3T3-L1 Cells, PLoS ONE 8(12):e82099, 2013. doi:10.1371/journal.pone.0082099.
- Axelsson J, et al: Effects of Sustained Sleep Restriction on Mitogen-Stimulated Cytokines, Chemokines and T Helper 1/T Helper 2 Balance in Humans, PLOS One 8(12):e82291, 2013.
- Kox M, et al: Voluntary activation of the sympathetic nervous system and attenuation of the innate immune response in humans, Proc Natl Acad Sci USA 111(20):7379–7384, 2014.

