A common complaint from folks on a vegan diet—especially newcomers—is that they are experiencing more gas and bloating since adopting the new way of eating. As you’ll soon see, this is a completely normal experience and can actually indicative of healthy processes taking place.
However, while the issue usually isn’t anything to be concerned about in terms of health, it can be quite uncomfortable especially when it persists for any length of time. And for this reason, I’ll be outlining some measures you can take to mitigate uncomfortable, rumbly sounds and sensations.
What we’ll do here is get into the main reasons people experience an increase in gas and bloating upon switching to the vegan diet, and what can be done to address each issue.
Food Intolerances: The Primary Cause of Initial Gas on the Vegan Diet
Food intolerances, known medically as adverse reactions to food (ARFs), are reactions that result in clinical symptoms, yet are not caused by an immune system reaction. This is to be distinguished from allergic reactions.
Adverse reactions to food take place in proportion to the amount of symptom-inducing foods eaten. Though I don’t like the framing, “adverse” due to the beneficial nature of some of the reactions covered here, gas production induced by a high-fiber vegan diet does fall into this area along with lactose intolerance, etc.
While ARFs are dose-dependent, allergic reactions are uncompromising. I.e. whereas for someone with lactose intolerance, a little milk results in a little gas, when someone is strongly allergic to a food, a tiny bit of the offending food results in an all-out assault.
The ingested compounds end up on the most wanted list and are targeted relentlessly by the immune system. For this reason, allergic reactions are much more serious, because immune-mediated responses in the body can cause life-threatening anaphylactic reactions—a feature not shared by ARFs.
As mentioned above, adverse reactions to food take place via nonimmunologic mechanisms.
These include:1
- Pharmacologic mechanisms (drugs)
- Toxicity
- Genetic factors
- Metabolic factors
- Psychogenic factors
- Gastrointestinal mechanisms
- And finally idiosyncratic, or idiopathic reactions (subjective symptoms for which there are no known explanations).
That’s a ton of categories, and as you might imagine, food intolerances are much more commonplace than food allergies. They’re usually triggered by small molecular weight chemicals and bioactive food components.1
The symptoms caused by food intolerances and those caused by allergic reactions can actually be quite similar—remember, the main difference is that food intolerances are dose-dependent.
Shared symptoms include:1
- GI manifestations (bloating and gas)
- Respiratory symptoms (difficulty breathing)
- Neurological manifestations (headaches)
- Skin manifestations (breakouts)
In the section on food intolerances, I’ll just be briefly covering what’s most relevant to the topic of gas and bloating.
An Ironic Truth: Why Gas Due to the Vegan Diet Can Actually Be a Good Thing
Carbs can slip past the small intestine into the large intestine. This is because specific carbs have certain chemical bonds that can’t be broken down by the enzymes in our small intestine. Namely fiber, and resistant starch.
We may not have the needed enzymes to break these carbs down, but certain bacteria in our large intestine do.
The bacteria that have the needed enzymes are in many cases thought of as “good bacteria.” There are certain species of bacteria that just love to snack on these carbs.
The results are two-fold:
- First, they create what are thought to be beneficial byproducts—what are known as short-chain fatty acids (SCFAs) like propionate. Human data are lacking, but they’re thought to be able to blunt appetite, improve insulin resistance, among providing many other benefits.2,3
- Secondly, the healthy microbes are being fed by these carbs which allows them to grow in number. When they receive a needed fuel source, they can multiply, grow in quantity, and create a healthy environment in the gut—one that lowers the risk of colon cancer.4
In her wonderful book Vegan for Life, Virginia Messina aka the Vegan RD sums it up well:
“New vegans who aren’t used to eating legumes and high-fiber foods may experience another type of intolerance that results from increased gas production and intestinal discomfort. It’s hard to convince people that gas is good for them, but it may very well be true!”5
Problem: Carbohydrate Intolerance
This is the category of food intolerances that’s most relevant to the vegan diet. When I say carbohydrate, I’m not just talking about plain old glucose, but all forms of carbs, especially those making up the FODMAP category which stands for “fermentable oligo-, di-, mono-saccharides and polyols.”6
Why Do High Carb Vegan Foods Make Me Gassy And Bloated?
The GI-related food intolerances potentially induced by the vegan diet are mostly related to carbohydrate consumption—sugars, starches, and fibers.
The sequence looks like this:
- Unabsorbed carbs in the small intestine eventually hit the colon still intact.
- These carbs together with water due to the osmotic effect (because carbs love water) can increase the osmotic load with tons of water in the GI tract (a fancy way of saying it leads to bloating).7
- Your gut bugs ferment these unabsorbed carbs making gas in the process (hydrogen, CO2 and methane) which leads flatulence and more bloating.8
How Do They Get to the Colon Undigested? Don’t We Have Enzymes?
Yes, carbs need to be broken down via enzymes in the small intestine to be absorbed and assimilated.
“Adverse” (potentially beneficial, yet unpleasant) reactions occur when carbs slip past the small intestine in one piece.
This happens for two primary reasons.
Enzyme Deficiency
There is a deficiency of enzymes responsible for breaking down certain types of carbohydrates, specifically disaccharides (e.g. lactose or sucrose). There’s not enough around to disassemble all the carbs, so a lot of the carbs make it to the large intestine.
Low production of specific enzymes can be the problem—as in the case of lactose intolerance. Many people don’t have enough of the enzyme lactase which is needed to break down lactose, and when the lactose hits the colon, the bacteria present in the large bowel—which do have the needed enzymes—abruptly begin to digest the sugars unleashing a ton of gas in the process.
See, non-vegans have their problems with digestion too, and thankfully lactose intolerance isn’t a problem vegans have to deal with.
And then there are the carbs for which our SI lacks the enzymes altogether (FODMAPs).
Vegans who aren’t used to eating legumes and other high-fiber foods will probably experience this type of intolerance resulting in increased production of gas and GI discomfort.
Malabsorption
There’s malabsorption of the breakdown products. I.e. there are plenty of enzymes available to break down the carbs, but once broken down they’re not absorbed for whatever reason and are passed on to the colon. Now you have a bunch of digested carbs (glucose, etc.) in the large intestine.
Remedies
Start Small with High Fiber Foods
As healthy bacteria proliferate in the gut, it should result in less gas production over time. When I first transitioned to a vegan diet—rather abruptly—I experienced some uncomfortable GI symptoms.
Fortunately, by that time I’d come to understand the important role of fiber in gut health. For this reason, I decided to just be patient and wait it out, knowing that symptoms would improve with time.
I started with a low dose of beans, and increase it over time. At first, it was 1/8 of a cup, then 1/4, 1/2, and so on. I’m now at the point where I can comfortably eat 2 cups of beans in one sitting.
If You Want to Consume Legumes, Start with Lentils
For whatever reason, lentils are known to induce much less gas than other beans. So, when first starting out, you may want to begin your high-fiber journey with lentil beans, and eventually, introduce different types of legumes over time.
Soak Your Beans
When you soak and rinse beans before cooking them, it removes a significant amount of fermentable, undigestible sugars. So, don’t forget to soak, soak, soak.
Exogenous Enzymes (Beano, Etc.)
You probably know that there are pills one can take for lactose intolerance (Lactaid). Well, there are also supplements that you can take to reduce unpleasant symptoms from eating beans. Beano is the most popular.
Remember the mentioning of enzymes above? The bacteria in your large intestine have the correct enzymes to digest sugars, while your small intestine lacks these enzymes.
Well, you can take needed enzymes (specific to digesting beans) in the form of a pill, which helps you break down these sugars before they reach the bacteria in your colon.
Due to the benefits, I outlined above, I strongly recommend that you try the other methods before resorting to enzymes.
Or alternatively, you could take them in the beginning, and just reduce the dose (of enzymes) over time. In this way, you will ultimately be able to reap the benefits of a high fiber diet on your gut ecosystem, while minimizing unpleasant side effects.
Problem: Allergies and Other Common Food Intolerances
Again, ARFs encompass the following:
- Food allergies. Reactions with an immunological basis that result from ingesting certain proteins.
- Food intolerance. Adverse reactions to food that don’t involve the immune system. These occur due to reactions to certain chemicals, as well as enzyme deficiencies, etc.
Both categories of ARFs are known to cause gas and bloating and food intolerances are the most common.9
We’ll focus on plain old food intolerances because only a few ARFs account for true IgE-mediated food hypersensitivity. Also, true food allergies are severe and often life-threatening, so if you have any, chances are you’ve known about it for most of your life.
Histamine Intolerances
This is a common cause of gas and bloating on the vegan diet.
Histamine intolerance occurs when there’s a buildup of the compound histamine in the body. We all have a certain level of histamine that we can tolerate without symptoms, but when levels exceed this threshold, symptoms occur.
Anyway, the histamine content in common foods (many being plant-based) has long been implicated as a primary cause of food intolerances that lead to gas and bloating.10
Histamine-rich foods can be of animal origin (e.g. tuna and cheese), but several plant-based foods contain high levels of the compound.
These include:11
- Bananas
- Strawberries
- Most citrus fruits
- Pineapple
- Tomatoes
- Peanuts
- Certain greens like spinach
- Green tea
- Legumes like chickpeas, soybeans, and lentils
- Sauerkraut
- Cocoa powder and chocolates
- Sweets containing preservatives
- Alcohol—some alcoholic beverages can contain upwards of 500 mg/kg of histamine
- Vinegar
Remedy: Food/Symptom Records and Elimination Diets
If food intolerances are the culprit, you’ll need to consult with a doctor, and preferably with a registered dietitian (RD).
Medical Nutrition Therapy (MNT) often involves:
- A thorough history.
- An assessment of any medical conditions you currently have, as well as any medications or dietary supplements you are taking.
- Lifestyle factors.
- A nutrition-focused physical assessment (NFPA).
Food records are usually performed with a 7-14 day food and symptom journal where you’ll be asked to log everything you eat along with any accompanying symptoms.
With food elimination diets, the suspect problem foods are completely taken out of the diet for anywhere from 4 to 12 weeks, at which point you’ll be instructed to reintroduce the foods in a controlled manner while monitoring for symptoms
Other Tips
Avoid “Aerophagia”

This is not really a food intolerance, but it is related to food intake and often causes gassy symptoms. Aerophagia is the swallowing of air. It’s done either accidentally, deliberately (to induce belching), or as an involuntary habit.
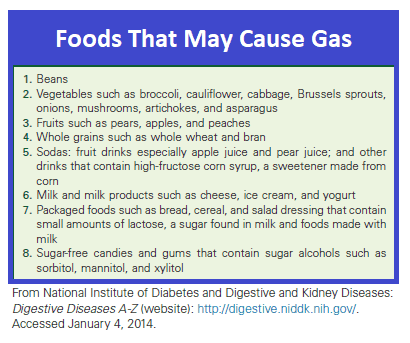
Stuff that can lead to aerophagia include:12
- Eating and drinking too quickly
- Chewing gum
- Using a straw when drinking
- Consuming carbonated beverages
- Smoking
- Loose dentures
Caffeine Caution
We all know what caffeine is, and what the common sources are—coffee, tea, sports drinks, and many soft drinks. It’s also added to some pharmacological products, like painkillers, cold/flu, diuretics, anti-histamine preparations, weight-loss products, and energy supplements.
It can be somewhat problematic because as a stimulant, it messes with colonic motility and it does cause gas and bloating for many people. But a lot of folks tolerate caffeine just fine, and it definitely varies from person to person.13
I am picking on caffeine, but this really applies to stimulants in general. Interestingly, the consumption of coffee increases colonic motility and stimulates the need to defecate in 29% of people whether or not the coffee contains caffeine.14,15
Even if you’ve always consumed caffeine and typically tolerate it well, if it gives you any problem at all, it may be best to moderate your intake.
At least while you’re transitioning to the vegan diet. You really don’t need the added food intolerance right now.
Limit Artificial Sweetened Products
Sugar-free food products like candies and gum often have problematic sugar alcohols like Mannitol, Sorbitol, and Xylitol.
Sorbitol is a poorly absorbed sugar alcohol that’s naturally found in some fruit in small amounts but is added in large amounts to reduced-sugar or sugar-free products—soft drinks, chewing gum, etc.16
Problem: Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome (IBS) is a condition characterized by unexplained abdominal discomfort and pain associated with changes in bowel movements.
IBS-associated GI symptoms (including gas and bloating) are thought to be associated with GI motility disturbances, visceral hyperactivity, sugar malabsorption, altered intestinal permeability, and gas-handling disturbances.17,18
Non-absorbable sugars (e.g. lactulose) are thought to exacerbate gaseous distention in folks with IBS.19
Altered motility is thought to play a role because when food makes its way through the intestines too quickly, the food content has less exposure to enzymes which causes malabsorption, gas, and bloating.20
Remedy: MNT and Low-FODMAP Diets
Vegans with IBS must consult a physician and RD to for customized diet therapy. The goals of IBS therapy are to tailor the diet per the specific GI pattern of IBS and ensure adequate intake of essential nutrients.
MNT typically involves the following:21
- Review of current medications and dietary supplements (herbs, probiotics, vitamins, and minerals, etc.)
- Review of GI symptoms the patient is experiencing (frequency, duration, and severity)
- Assessment of nutritional status and food intake
- Review of any alternative or mind-body therapies the patient may be using
Food components that are typically monitored due to their association with gas and bloating in IBS include FODMAPs, caffeine, sorbitol, and alcohol.22
The low-FODMAP diet has long been considered effective in managing GI symptoms in IBS.23
Patients with IBS are often put on a low FODMAP diet, but it’s advised that one do this under the instruction of an RD.
Recent studies have shown certain carb-containing foods to worsen IBS symptoms like gas and bloating, specifically carbs that are highly fermentable.24
The FODMAP diet limits short-chain carbohydrates (di-, tri-, and oligosaccharides) because they are poorly absorbed in the SI, and due to their highly osmotic (water-attracting) properties. They are rapidly fermented by colonic bacteria which leads to gas and bloating, and other GI symptoms like diarrhea and stomach pain.
Specifically, the FODMAP diet limits foods that contain:22
- Fructo-oligosaccharides (fruits)
- Lactose—the simple sugar in milk (not a problem for vegans)
- Galacto-oligosaccharides (common legumes)
- Polyols or sugar alcohols (mannitol, xylitol, sorbitol, maltitol, and isomaltase)
Again, this type of thing needs to be done under the supervision of a medical professional. RDs help IBS patients navigate the low-FODMAP diet because if done poorly, it can lead to nutrient deficiencies (e.g. thiamine, folate, B6).
Problem: Irritable Bowel Disease (IBD)
Inflammatory bowel disease (IBD) is an umbrella term for several conditions that result in bowel inflammation—namely Crohn’s disease (CD) ulcerative colitis (UC), though other disorders are included in this category (microscopic/lymphocytic colitis, diverticulitis, etc.).
Both CD and UC involve a multi-system group of overlapping symptoms and present with their own clinical manifestations. They’re both known for intermittent periods of elevated/worsened symptoms followed by stretches of time where they seem to be in remission—either in response to treatments or spontaneously.
UC involves inflammation of the mucosa in the colon and rectum. The inflammation often starts in the rectum and progresses proximally from there.25
In contrast, CD often involves inflammation that spans the entire GI tract, but the inflammation can present as pure colitis.26
Gas and bloating are among the most common symptoms in folks with IBD and the resulting discomfort can range from a mere annoyance to a life-threatening crisis.27
While the two conditions are similar, the main differences between CD and UC are important because they determine the manifestation of their symptoms. For example, while diarrhea is the initial symptom in nearly all cases of UC, it’s the initial symptom in only about 50% of flares in CD.28
However, gas and bloating are two of the most common manifestations in both.
Remedy: Medical Management and MNT
At present, there aren’t any specific dietary protocols that are recommended across the board for patients with UC and CD.29
Because not all patients with IBD present with the same symptoms, the therapy is always tailored according to the etiology.27
However, there are some general measures that tend to be recommended for folks with IBD.
These include:29,30
- The use of well-tolerated foods
- Minimizing fiber intake
- Eating smaller and more frequent meals if gas and bloating are a problem
- Tests for food intolerances—caffeine, fructose and non-absorbable carbs like artificial sweeteners.
Problem: Small Intestine Bacterial Overgrowth (SIBO)
Small intestinal bacterial overgrowth, or SIBO, is a syndrome in which bacteria that normally inhabit the large intestine, makes its way into and takes up residence in the small intestine.
The over-proliferation of bacteria in the SI isn’t normal, and results in symptoms including gas and bloating. SI isn’t very hospitable to invading bacteria because your body has a number of processes in place to limit the number of bacteria in this section of the GIT.
For example, bile, gastric acid, and pancreatic enzymes all have bacteriostatic and bactericidal action that keeps the growth of these organisms in check.
For example, peristalsis (the propulsive action of the intestines) moves both food and bacteria into the distal bowel.
Then there’s what’s known as the ileocecal valve which prevents retrograde migration of colonic bacteria into the small intestine.
Another term for SIBO is “blind loop syndrome” because bacterial overgrowth in the SI can result from intestinal stasis due to obstructive disease, intestinal strictures, surgical procedures and radiation enteritis—a group of conditions that all leave a section of the intestines without normal flow (a Roux limb or blind loop).
Remedy: MNT and Dietary Modification
RDs and physicians focus primarily on dietary modification designed to correct nutrient deficiencies and alleviate symptoms.
In theory, diets that limit refined rapidly-fermenting carbs (namely sugars, starches, and sugar alcohols), replacing them with veggies and whole grains should be helpful, as this eating pattern is thought to increase gut motility and limit bacterial proliferation.31
One of the problems with SI bacterial overgrowth is that when carbs reach the site where microbes have accumulated, the result is a full-on feeding frenzy that produces gas and organic acids. For this reason, carbohydrate consumption is often the focus of treatment.
That’s it for gas and bloating. Thanks for reading.
You may also want to check out the following related articles:
- The Vegan Diet and Diarrhea (Causes, Remedies)
- The Vegan Diet and Constipation: Everything You Need to Know
- The Vegan Diet and Hemorrhoids
References
- Krause’s Food & the Nutrition Care Process (Page 487) L. Mahan-Janice Raymond – Elsevier – 2017
- C S Byrne, E S Chambers, D J Morrison, The role of short-chain fatty acids in appetite regulation and energy homeostasis. Int J Obes (Lond). 2015;39(9): 1331–1338 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4564526/
- Hur K.Y., Lee M.-S. Gut microbiota and metabolic disorders. Diabetes Metab. J. 2015;39:198–203.
- Gropper, Sareen S.; Smith, Jack L.. Advanced Nutrition and Human Metabolism (Page 122).
- Virginia Messina and Jack Norris. Vegan for Life: Everything You Need To Know To Be Healthy (Page 94). ISBN: 978-0-7382-1493-1
- Peter R Gibson, Susan J Shepherd. Evidence‐based dietary management of functional gastrointestinal symptoms: The FODMAP approach. https://onlinelibrary.wiley.com/doi/full/10.1111/j.1440-1746.2009.06149.x
- Cummings JH, Macfarlane GT. The control and consequences of bacterial fermentation in the human colon. J Appl Bacteriol 1991; 70: 443–59.
- AY Seo, Nayoung K, and Dong HO, Abdominal Bloating: Pathophysiology and Treatment. J Neurogastroenterol Motil. 2013;19(4): 433–453. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3816178/
- Cochrane S, Beyer K, Clausen M, Wjst M, Hiller R, Nicoletti C, Szepfalusi Z, Savelkoul H, Breiteneder H, Manios Y, Crittenden R, Burney P. Factors influencing the incidence and prevalence of food allergy. Allergy 2009;64(9): 1246–1255.
- Wöhrl S, et al. Histamine intolerance-like symptoms in healthy volunteers after oral provocation with liquid histamine. Allergy Asthma Proc. 2004 Sep-Oct;25(5):305-11.
- Jee Hee Son, et al. A Histamine-Free Diet Is Helpful for Treatment of Adult Patients with Chronic Spontaneous Urticaria. Ann Dermatol. 2018 Apr; 30(2): 164–172. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5839887/#S1
- Krause’s Food & the Nutrition Care Process (Page 526) L. Mahan-Janice Raymond – Elsevier – 2017
- Boekema PJ, Samsom M, van Berge Henegouwen GP, Smout AJ. Coffee and gastrointestinal function: facts and fiction. A review. Scand J Gastroenterol Suppl 1999; 230: 35–9.
- Brown SR, Cann PA, Read NW. Effect of coffee on distal colon function. Gut 1990; 31: 450–3.
- Rao SS, Welcher K, Zimmerman B, Stumbo P. Is coffee a colonic stimulant? Eur J Gastroenterol Hepatol 1998; 10: 113–18.
- Rumessen JJ. Fructose and related food carbohydrates: sources, intake, absorption, and clinical implications. Scand J Gastroenterol 1992; 27: 819–28.
- Drossman DA, Corrazziari E, Delvaux M, Spiller R, Talley NJ, Thompson WG. Rome III: The Functional Gastrointestinal Disorders. McLean, VA: Degnon Associates; 2006.
- Review Diagnosis of irritable bowel syndrome. Cash BD, Chey WD Gastroenterol Clin North Am. 2005 Jun; 34(2):205-20, vi.
- Lekha Saha. Irritable bowel syndrome: Pathogenesis, diagnosis, treatment, and evidence-based medicine. World J Gastroenterol. 2014 Jun 14; 20(22): 6759–6773. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4051916/
- Schiller LR, Sellin JH. Diarrhea. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran’s gastrointestinal and liver disease: pathophysiology, diagnosis, management, 8th edn (Ed. Feldman M) Philadelphia: WB Saunders; 2006. pp. 159–186.
- ME, Ireton-Jones C: Irritable bowel syndrome: new frontiers in treatment, Support Line 34(6):8, 2012.
- Krause’s Food & the Nutrition Care Process (Page 547). L. Mahan-Janice Raymond – Elsevier – 2017
- Halmos EP, Power VA, Shepherd SJ, et al: A diet low in FODMAPs reduces symptoms of irritable bowel syndrome, Gastroenterology 146:67, 2014.
- Mullins GE, Shepherd SJ, Chander Roland B, et al: Irritable bowel syndrome: contemporary nutrition management strategies, J Parenter Enteral Nutr 38:781, 2014.
- Diarrhea Diagnostic and Therapeutic Advances (Page 62). Stefano Guandalini-Haleh Vaziri – Humana Press – 2011
- Lichtenstein G, Hanauer S, SandbornW, the Practice Parameters Committee of the American College of Gastroenterology. Management of Crohn’s disease in adults. Am J Gastroenterol 2009;104:465–483.
- Shah S, Hanauer S. Treatment of diarrhea in patients with inflammatory bowel disease: concepts and cautions. Gastroenterol Disord 2007;7(Suppl 3):S3–S10.
- Kucharzik T,Maaser, C, Lügering A, et al. Recent understanding of IBD pathogenesis: implications for future therapies. Inflamm Bowel Dis 2006;12:1068–1083.
- Diarrhea Diagnostic and Therapeutic Advances (Page 77). Stefano Guandalini-Haleh Vaziri – Humana Press – 2011
- Krause’s Food & the Nutrition Care Process (Page 543). L. Mahan-Janice Raymond – Elsevier – 2017
- Krause’s Food & the Nutrition Care Process (Page 552). L. Mahan-Janice Raymond – Elsevier – 2017