Like gas/bloating, constipation and hemorrhoids, diarrhea (or just the occasional loose stool) is another digestive issue folks can face when switching to plant-based diets.
The World Health Organization (WHO) defines diarrhea as the passage of three or more liquid or loose stools per day.1 The stool is liquid or loose because diarrhea is due to excessive fluid in the gastrointestinal tract (GIT).
Diarrhea can be classified in a number of ways (acute vs. chronic, etc.). In Krause’s Food & the Nutrition Care Process, Gail Cresci and Arlene Escuro lay out a few of the main categories of diarrhea.2
- Malabsorptive diarrhea. Impaired digestion and absorption of nutrients create osmotic pressure that pulls water into the GIT. Diet definitely comes into play here as the overconsumption of sugars and other osmotic substances can cause this type of diarrhea.
- Osmotic diarrhea. Like malabsorptive diarrhea, this kind results from osmotically active solutes in the intestines that pull water in. Diarrhea classified as osmotic isn’t necessarily a result of malabsorption.
- Secretory diarrhea. Infections with bacterial, fungal, or viral agents can cause this type of diarrhea. When you get an infection, your body dumps a bunch of fluid into your intestines to flush it out. This one can also be diet-related (food poisoning, etc.).
- Exudative diarrhea. Often due to inflammatory disease. The damaged mucosal area triggers the flow of fluids into the intestines. Food intolerances (gluten, etc.) can trigger this type of diarrhea.
- Medication-induced diarrhea. Some medications are known to cause diarrhea and by different mechanisms like increasing bowel movements as part of their main function.
As you can see, diet is not implicated in all of the causes, so what we’ll do is cover the above etiologies that relate to plant-based eating.
Quick note: one question I get asked quite a bit is whether there are any specific “superfoods” that are known to be helpful in preventing/alleviating diarrhea.
One food in particular, the tamarind, is thought to potentially alleviate diarrhea and dysentery.
The pulp with lemon is used to treat diarrhea, while the root is commonly used to treat dysentery.39,40,41
But, there’s very little research in this area and when it comes to digestive issues, the focus should really be on addressing the underlying cause, more so than relying on a specific food product.
Problem 1: Low Protein Intake
Remember, the WHO defines diarrhea as three or more loose or liquid stools per day. Another problem folks can run into is just having more loose stools than usual, which may not rise to the level of clinically defined diarrhea.
This isn’t really a matter of protein per se. The effect of low protein intake on stool consistency is really just the flip side of the effect of low fiber intake on constipation.
In Vegetarian and Plant-based Diets in Health and Disease Prevention, authors state, “A high intake of fiber tends to reduce the absorption of minerals and increases the risk of diarrhea.”3 Fiber aids water retention in the colon and results in moist stools that are easier to evacuate.4 So if you eat a lot of fruit and little else then it wouldn’t be surprising that your stool lacked firmness.
If you’ve ever seen the old hit show LOST you may remember that watery stool turned out to be an issue for many of the castaways. Hurley complained to Jack (the resident doctor) that he was having issues and Jack immediately asked what he was eating. Hurley’s diet of nearly 100% mango had quite the effect on stool consistency.
A lot of raw vegans are near-fruitarians if not full on fruitarians. Many in this group eat lots of fruit and nuts and not much else. This is a recipe for loose stool. Raw food vegan or not, folks on plant-based diets are notorious for neglecting protein intake and as a result, fiber tends to fill the void.
Remedy
Ensure adequate protein intake.
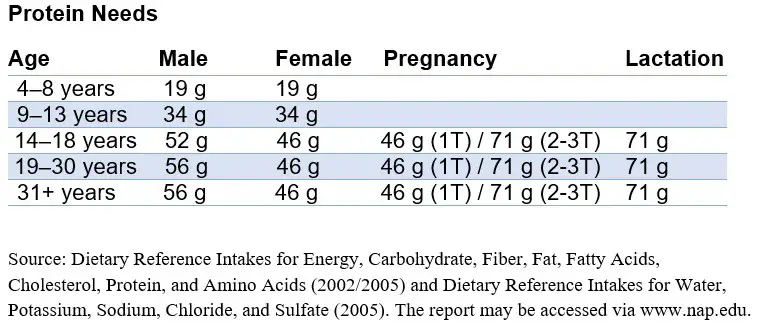
Currently, the Recommended Dietary Allowance (RDA) for protein for adults (both men and women 19 years of age and older) is 0.8 g of protein per kg of body weight per day.5
I wrote an extensive article on all the best sources of vegan protein you can read here.
Problem 2: Micronutrient Deficiency
Zinc Deficiency
Severe zinc deficiency can lead to diarrhea among other symptoms such as immunologic deficits, alopecia (hair loss), weight loss, emotional disorders, and hypogonadism (reduced physiological activity of the testis and ovaries).6
In fact, zinc is now included in the WHO’s essential medicine list for diarrhea treatment.7
What’s this have to do with the vegan diet? Well, human zinc deficiency was first recorded in the Middle East in young men who mostly consumed plant-based diets high in wheat and low in animal protein.8,9
Don’t get me wrong, you can get plenty of zinc outside of animal-protein sources. But, the mineral is known to be problematic for vegans and other plant-based eaters. Plant-based populations in low- and middle-income countires perhaps have the highest risk of diet-induced overt zinc deficiency, and many such people regularly experience diarrhea.10
Severe overt zinc deficiency is less common in plant-based eaters from high-income countries (HIC), but inadequate zinc intakes and chronic/mild zinc deficiency is very prevalent in these countries.11
In fact, vegetarians from high-income countries are among the populations having the highest risk of subclinical zinc deficiency. The mineral is less abundant in the plant kingdom and zinc from plant sources is less bioavailable compared with zinc found in animal food sources.12
Diarrhea is a common manifestation of zinc deficiency in both children and adults. Other populations are known to be at risk of zinc deficiency which would just compound the risk if the person happens to be vegan. Other populations include:13
- Elderly
- Children of low income
- Those with alcoholism
- Certain conditions—malabsorption, trauma, and sickle cell anemia
Remedy
Ensure adequate zinc intakes.
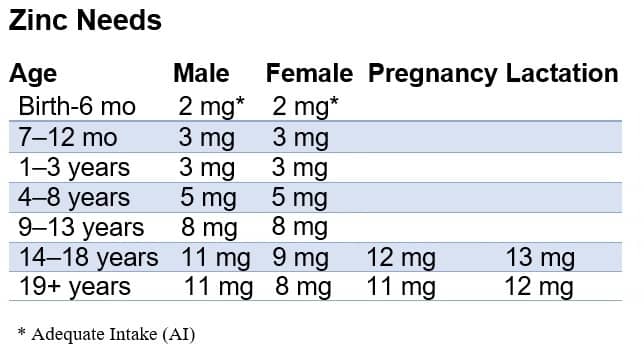
Source: Office Of Dietary Supplements – Zinc https://ods.od.nih.gov/factsheets/Zinc-HealthProfessional/
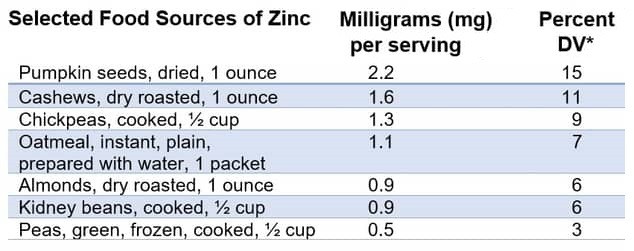
Source: Office Of Dietary Supplements – Zinc https://ods.od.nih.gov/factsheets/Zinc-HealthProfessional/
Other Nutrients
Deficiency of these nutrients is much less likely on plant-based diets, but diet composition among vegans can vary significantly so we’ll cover them just in case.
Niacin
Pellagra is a condition that develops with severe niacin deficiency. You may have heard of the Four D’s of Pellagra, and you guessed it, diarrhea is one of them.
GI manifestations of niacin deficiency also include glossitis (inflammation of the tongue), angular stomatitis (sores at the corners of the mouth), cheilosis, nausea and vomiting.14
Remedy
Ensure adequate niacin intakes.
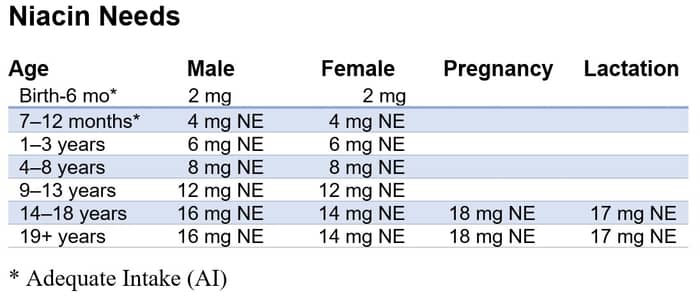
Source: Office Of Dietary Supplements – Niacin https://ods.od.nih.gov/factsheets/Niacin-HealthProfessional/
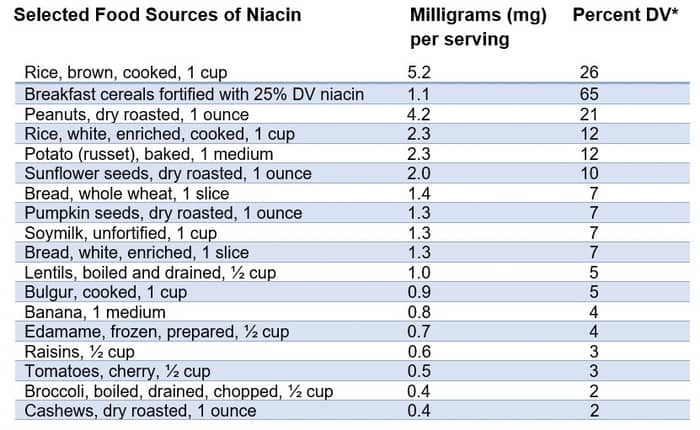
Source: Office Of Dietary Supplements – Niacin https://ods.od.nih.gov/factsheets/Niacin-HealthProfessional/
Folate
Again, folate deficiency is unlikely on a plant-based diet. It’s ubiquitous in the plant kingdom and many B vitamins, in general, are fortified out the wazoo. But, anything is possible and for the sake of completeness, we’ll touch on it here.
Severe folate deficiency results in impaired DNA synthesis affecting all cells, but most notably RBCs because they’re rapidly dividing. Other high-turnover cells include those of the GI tract. This results in digestive issues due to shortening of villi height which thins the layers of the intestines resulting in impaired nutrient absorption and diarrhea.15
Remedy
Ensure adequate folate intakes.
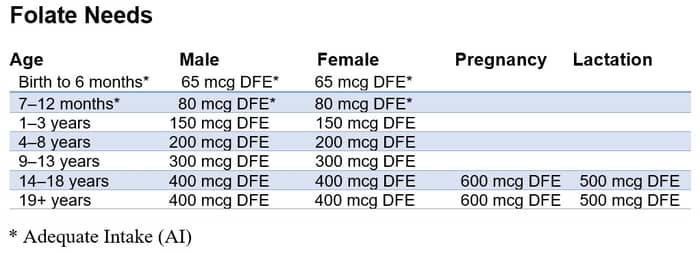
Source: Office Of Dietary Supplements – Folate https://ods.od.nih.gov/factsheets/Folate-HealthProfessional/
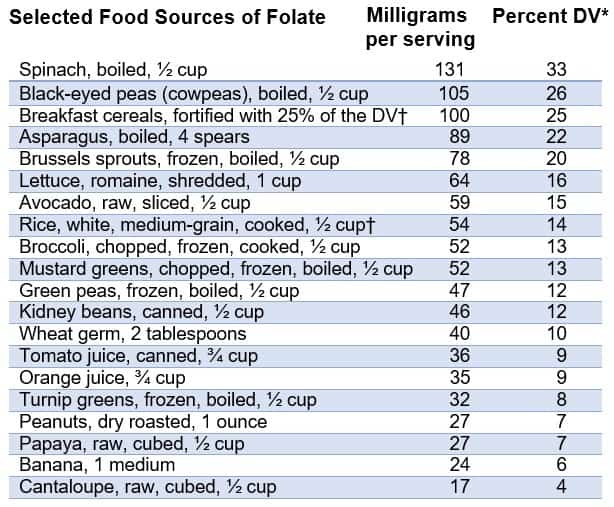
Source: Office Of Dietary Supplements – Folate https://ods.od.nih.gov/factsheets/Folate-HealthProfessional/
Problem 3: Supplementation
When switching to the vegan diet, people are often concerned about nutrient deficiencies. For this reason, some try to preempt inadequate intake by taking a ton of vitamin and mineral supplements many of which can cause diarrhea in excess.
Both the dosage and the form of the nutrient can determine how well it’s tolerated. For example, a lot of people tend to have problems with magnesium oxide. We talked above about how zinc deficiency can lead to diarrhea. Well, paradoxically, zinc supplementation often causes the same problem especially if taken in high amounts.
The effect of too much zinc isn’t limited to diarrhea and can include abdominal pain, nausea, vomiting, and dyspepsia.16
Problem 4: High Levels of Physical Activity
I hesitate to say excessive because PA is so good for you. But, I bring this one up because vegans tend to be an active bunch. If you read the article on constipation, you know that physical activity has long been an evidence-based approach to get things moving along. Well, lots of physical activity can trigger the opposite condition: diarrhea.
They call this “the runs” or “the trots.” I once knew a runner who always took a roll of toilet paper when out for long-distance runs. If you’ve taken a dog for a while, which I’m sure you have, you probably noticed that the physical movement tended to encourage pooping.
Vigorous activity, especially sprinting, is known to have a powerful stimulatory effect on bowel activity to the point of inducing diarrhea.
Remedy
Diagnosis and medical treatment.
It may sound straight-forward, but diagnosing runner’s diarrhea is complicated and there’s actually an entire algorithm for it.17
Treatment usually involves assessment of nutritional habits that may also be contributing to runner’s diarrhea.
Problem foods are thought to include:
- Sports drinks and carbohydrate-containing gels—especially those with concentrations exceeding 7 to 10% as they create a gradient that leads to osmotic diarrhea.18
- High-fiber and high glycemic index (GI) foods
- Caffeine—the compound is often used before long races due to its effects on fat metabolism. If you read the article on bloating, you know that caffeine exerts a laxative effect.17
Problem 5: Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome (IBS) is a condition that’s characterized by unexplained abdominal pain and discomfort associated with changes in bowel movements. IBS-associated diarrhea is thought to be due to altered colonic transit/motility and/or hypersensitivity of the rectum.19
Studies show that up to 60% of IBS patients may have rectal hypersensitivity, and this hypersensitivity seems to be more prevalent in diarrhea-predominant IBS.20,21
Inflamed mucosa is also implicated as a cause of diarrhea in IBS.22 Disordered motility in IBS is thought to cause both osmotic and secretory diarrhea.23
When food transits the intestines too quickly, there’s less exposure of the food content to enzymes which causes malabsorption.23
Remedy
MNT and low-FODMAP diets.
Folks with IBS must consult a physician and registered dietitian to get tailored diet therapy. The goals of IBS therapy are to ensure adequate intake of nutrients and customize the diet per the patient’s specific GI pattern of IBS.
MNT involves typically involves the following.24
- Review of current medications
- Review of GI symptoms (duration, frequency, severity)
- Assessment of food intake and nutritional status
- Review of any supplement intake (multivitamins, herbals, pre- and probiotics, etc.
- Review of any mind-body therapies used
Food components that are monitored/assessed in the diet due to their association with diarrhea-predominant IBS include:25
- Fructose
- Dietary fat
- Caffeine
- Sorbitol
- Alcohol
As for the low-FODMAP diet, recent studies have shown certain carbohydrate-containing foods to exacerbate IBS symptoms, specifically those that contain highly fermentable carbohydrates.26
It turns out the low-FODMAP diet may be effective in managing GI symptoms in IBS.27
The diet limits short-chain carbs that are poorly absorbed in the SI, as they are highly osmotic (attract water), and are rapidly fermented by gut bacteria which leads to diarrhea as well as gas, bloating, stomach pain, etc.
Specifically, the diet limits foods that contain:25
- Lactose (not a problem for vegans)
- Fructo-oligosaccharides (fruits)
- Galacto-oligosaccharides (legumes)
- Polyols or sugar alcohols (xylitol, mannitol, sorbitol, isomaltase, and maltitol)
Registered dietitians help IBS patients navigate the low-FODMAP diet to help avoid nutrient deficiencies that are common to this eating pattern (e.g. thiamine, folate, B6)
Problem 8: Food Allergies and Intolerances
Adverse reactions to food (ARF) is a term that encompasses the following:
- Food allergies—reactions to food proteins that have an immunological basis
- Food intolerance—adverse reactions to ingested food that don’t involve the immune system. Due to enzyme deficiencies, reactions to chemicals in food, etc.
Both types of ARFs are known to cause diarrhea with the latter (food intolerances) being the most common.28
We’ll focus on regular old food intolerances given that only a few ARFs represent a true food hypersensitivity via igE-mediated pathogenesis. Also, allergies are severe and can even be life-threatening, so if you have one you’ve likely known about it for most of your life.
Histamine Intolerances
Histamine intolerance happens when there’s a buildup of histamine in the body. Everyone has a level of histamine that can be tolerated, and when levels exceed that threshold, symptoms develop.
Anyway, the histamine in common foods has been implicated as a major cause of food intolerance causing GI symptoms like diarrhea.29
A lot of histamine-rich foods are of animal origin such as cheese and tuna, but several plant foods contain the chemical including.30
- Strawberries
- Bananas
- Tomatoes
- Sauerkraut
- Legumes like soybeans, chickpeas, and lentils
- Green tea
- Sweets containing preservatives
- Cocoa and chocolate
- Pineapple
- Most citrus fruits
- Spinach
- Peanuts
- Vinegar
- Alcohol—alcoholic beverages can contain up to 500 mg/kg of histamine.
Carb Intolerance (Fructose and Fructose Polymers)

You’ve probably heard of FODMAPs by now, an acronym that stands for fructo-, oligo-, di-, and monosaccharides and polyols. It’s quite common for people to experience maldigestion and malabsorption of these fructose molecules.
Fructose polymers can be a problem for anyone if eaten in excess. That’s because we humans lack the hydrolase enzymes needed to break the bonds of the fructose chains. Again, if eaten in excess most people will develop GI symptoms of which diarrhea can be one.31
For some folks, the fructose itself (the monosaccharide) can be problematic. For these individuals, table sugar (sucrose) and free fructose (as in HFCS) can cause GI symptoms.
Remedy
Food/symptom records and food-elimination diets.
If food intolerances are an issue, you’ll need to consult with a registered dietitian (RD) or physician.
Medical Nutrition Therapy (MNT) may involve:
- A thorough history
- An assessment of current medical conditions, medications, and dietary supplements
- Lifestyle factors, exercise habits, etc.
- A nutrition-focused physical examination
Food records use a 7-14 day food and symptom journal where they’ll have a patient log everything eaten along with any symptoms triggered by a given food choice. These have proven very useful for revealing ARFs.
This type of record can also uncover possible nutrient deficiencies which, as we’ve seen, can also affect diarrhea. They may also have you track stress, physical exercise, and sleep patterns.
Then there’s the elimination diet. With these diets, the suspect foods are completely eliminated from the diet for about 4 to 12 weeks, at which point they’ll have you reintroduce the foods in a controlled way while symptoms are monitored.
Problem 8: Small Intestine Bacterial Overgrowth (SIBO)
SIBO is a syndrome wherein the over-proliferation of bacteria normally inhabiting the large intestine finds its way into the small intestine taking up residence there. Normally, the SI isn’t very hospitable to these bacteria as your body has a number of physiologic processes in place to limit the number of bacteria in this region of the GIT.
For example, gastric acid, bile, and pancreatic enzymes all have bactericidal and bacteriostatic action which keep the growth of these organisms at bay. Peristalsis (the normal propulsive action of the intestines) serves to sweeps the bacteria into the distal bowel.
What’s known as the ileocecal valve serves to prevent retrograde migration of colonic bacteria into the SI. SIBO is often referred to as “blind loop syndrome” because overgrowth can result from intestinal stasis due to strictures, obstructive disease, surgical procedures and radiation enteritis—conditions that leave a portion of the intestines without normal flow (a Roux limb or blind loop).
Remedy
MNT and dietary modification.
Physicians and RDs focus dietary modification on correcting nutrient deficiencies and alleviating symptoms.
Carbohydrate consumption is often the focus because one of the problems with bacterial overgrowth in the SI is that when ingested carbs reach the site where microbes are harbored it results in a full-on feeding frenzy which produces gas and organic acids.
Theoretically, diets limiting refined rapidly-fermenting carbohydrates (namely starches, sugars, and sugar alcohols), and replacing them with whole grains and veggies should be helpful by limiting bacterial proliferation and increasing gut motility.32
Problem 9: Irritable Bowel Disease (IBD)
Inflammatory bowel disease (IBD) is an umbrella term for a number of conditions resulting in inflammation of the bowels, namely ulcerative colitis (UC) and Crohn’s disease (CD), though other disorders fall under this category (diverticulitis, microscopic/lymphocytic colitis, etc.
Both UC and CD involve a multi-system group of symptoms with their own clinical features and are known for intermittent periods of exacerbated symptoms followed by periods of remission—either spontaneously, or in response to treatments.
Ulcerative colitis involves mucosal inflammation in the rectum and the colon, with the inflammation often starting in the rectum and progressing proximally from there.33 Crohn’s disease often involves inflammation spanning the entire GI tract, but can present as pure colitis.34
Diarrhea is one of the most common symptoms in patients with IBD and can range from an annoyance to a life-threatening crisis.35
The differences between UC and CD are important because they impact the manifestation of their symptoms. Diarrhea is the initial symptom nearly 100% of the time in UC and the initial symptom in about 50% of flares in CD.36
Remedy
Medical management and MNT.
Currently, there are no specific dietary protocols that are recommended across the board for patients with IBD.37
Because not all diarrheas in those with IBD present the same, the therapy has to be tailored according to the etiology.35
General measures that are taken include:37,38
- Use of well-tolerated foods
- Minimization of fat (esp. in those with fat malabsorption or ‘steatorrhea’)
- Minimizing fiber intake
- Eating smaller, more frequent meals if gas and bloating are a problem
- Prebiotics and probiotics are sometimes used
- Tests for food intolerances—fructose, non-absorbable carbohydrates like artificial sweeteners, and stimulants (caffeine)
Conclusion
This may have been a long article, but it barely scratches the surface. There are tons of reasons one might have diarrhea, many of which have nothing to do with diet—infections, etc. Always consult your doctor for diagnosis and treatment of any issues you may be having. I hope you learned a thing or two and for similar content check out the articles on bloating/gas, constipation, and hemorrhoids.
References
- Diarrhoeal Disease https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease
- Krause’s Food & the Nutrition Care Process (Page 528). L. Mahan-Janice Raymond – Elsevier – 2017
- Vegetarian and Plant-based Diets in Health and Disease Prevention (Page 534). François Mariotti – Elsevier Academic Press – 2017
- Kok-Sun Ho. Stopping or reducing dietary fiber intake reduces constipation and its associated symptoms. World J Gastroenterol. 2012 Sep 7; 18(33): 4593–4596.
- Food and Nutrition Board. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Protein and Amino Acids. Washington, DC: National Academy Press. 2002.
- Foster, M., Herulah, U.N., Prasad, A., Petocz, P., Samman, S., June 5, 2015. Zinc status of vegetarians during pregnancy: a systematic review of observational studies and meta-analysis of zinc intake. Nutrients 7 (6), 4512–4525.
- WHO Model List of Essential Medicines 18th list. https://www.who.int/medicines/publications/essentialmedicines/18th_EML.pdf
- Prasad, A.S., et al., 1963. Zinc metabolism in patients with the syndrome of iron deficiency anemia, hepatosplenomegaly, dwarfism, and hypognadism. J. Lab. Clin. Med. 61, 537–549.
- Prasad, A.S., Halsted, J.A., Nadimi, M., 1961. Syndrome of iron deficiency anemia, hepatosplenomegaly, hypogonadism, dwarfism and geophagia. Am. J. Med. 31 (4), 532–546.
- Samman, S., 2012. Zinc. In: Mann, J., Truswell, S. (Eds.), Essentials of Human Nutrition. Oxford University Press, Oxford.
- Wuehler, S.E., Peerson, J.M., Brown, K.H., 2005. Use of national food balance data to estimate the adequacy of zinc in national food supplies: methodology and regional estimates. Public Health Nutr. 8 (7), 812–819.
- Craig, W.J., Mangels, A.R., 2009. Position of the American dietetic association: vegetarian diets. J. Am. Diet. Assoc. 109 (7), 1266–1282.
- Gropper, Sareen S.; Smith, Jack L.. Advanced Nutrition and Human Metabolism (Page 509).
- Gropper, Sareen S.; Smith, Jack L.. Advanced Nutrition and Human Metabolism (Page 333).
- Gropper, Sareen S.; Smith, Jack L.. Advanced Nutrition and Human Metabolism (Page 352).
- Gropper, Sareen S.; Smith, Jack L.. Advanced Nutrition and Human Metabolism (Page 501).
- Ho GWK. Lower gastrointestinal distress in endurance athletes. Curr Sports Med Rep 2009;8(2):85–91.
- Rehrer NJ, Janssen GM, Brouns F, et al. Fluid intake and gastrointestinal problems in runners competing in a 25-km race and a marathon. Int J Sports Med 1989;10(Suppl 1):S22–S25.
- Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology 2002;123:2108–2131.
- Mertz H, Naliboff B, Munakata J, Niazi N, Mayer EA. Altered rectal perception is a biological marker of patients with irritable bowel syndrome. Gastroenterology 1995;109:40–52.
- Prior A, Colgan SM, Whorwell PJ. Changes in rectal sensitivity after hypnotherapy in patients with irritable bowel syndrome. Gut 1990;31:896–898.
- Chadwick VS, Chen W, Shu D, et al. Activation of the mucosal immune system in irritable bowel syndrome. Gastroenterology 2002;122:1778–1783.
- Schiller LR, Sellin JH. Diarrhea. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran’s gastrointestinal and liver disease: pathophysiology, diagnosis, management, 8th edn (Ed. Feldman M) Philadelphia: WB Saunders; 2006. pp. 159–186.
- Caldwell ME, Ireton-Jones C: Irritable bowel syndrome: new frontiers in treatment, Support Line 34(6):8, 2012.
- Krause’s Food & the Nutrition Care Process (Page 547). L. Mahan-Janice Raymond – Elsevier – 2017
- Mullins GE, Shepherd SJ, Chander Roland B, et al: Irritable bowel syndrome: contemporary nutrition management strategies, J Parenter Enteral Nutr 38:781, 2014.
- Halmos EP, Power VA, Shepherd SJ, et al: A diet low in FODMAPs reduces symptoms of irritable bowel syndrome, Gastroenterology 146:67, 2014.
- Cochrane S, Beyer K, Clausen M, Wjst M, Hiller R, Nicoletti C, Szepfalusi Z, Savelkoul H, Breiteneder H, Manios Y, Crittenden R, Burney P. Factors influencing the incidence and prevalence of food allergy. Allergy 2009;64(9): 1246–1255.
- Wöhrl S, et al. Histamine intolerance-like symptoms in healthy volunteers after oral provocation with liquid histamine. Allergy Asthma Proc. 2004 Sep-Oct;25(5):305-11.
- Jee Hee Son, et al. A Histamine-Free Diet Is Helpful for Treatment of Adult Patients with Chronic Spontaneous Urticaria. Ann Dermatol. 2018 Apr; 30(2): 164–172. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5839887/#S1
- Joneja JV: The health professional’s guide to food allergies and intolerances, Chicago, IL, 2013, Academy of Nutrition and Dietetics
- Krause’s Food & the Nutrition Care Process (Page 552). L. Mahan-Janice Raymond – Elsevier – 2017
- Diarrhea Diagnostic and Therapeutic Advances (Page 62). Stefano Guandalini-Haleh Vaziri – Humana Press – 2011
- Lichtenstein G, Hanauer S, SandbornW, the Practice Parameters Committee of the American College of Gastroenterology. Management of Crohn’s disease in adults. Am J Gastroenterol 2009;104:465–483.
- Shah S, Hanauer S. Treatment of diarrhea in patients with inflammatory bowel disease: concepts and cautions. Gastroenterol Disord 2007;7(Suppl 3):S3–S10.
- Kucharzik T,Maaser, C, Lügering A, et al. Recent understanding of IBD pathogenesis: implications for future therapies. Inflamm Bowel Dis 2006;12:1068–1083.
- Diarrhea Diagnostic and Therapeutic Advances (Page 77). Stefano Guandalini-Haleh Vaziri – Humana Press – 2011
- Krause’s Food & the Nutrition Care Process (Page 543). L. Mahan-Janice Raymond – Elsevier – 2017
- Santosh Singh Bhadoriya, et al. Tamarindus indica: Extent of explored potential. Pharmacogn Rev. 2011 Jan-Jun; 5(9): 73–81. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3210002/
- Kerharo J, Bouquet A. Paris: Vigot Freres; 1950. Plantes Médicinales et Toxiques de la Côte d′Ivoire et Haute-Volta.
- Chhabra SC, Mahunnah BLA, Mshiu EN. Plants used in traditional medicine in eastern Tanzania. I. Pteridophytes and angiosperms (Acanthaceae to Canellaceae) J Ethnopharmacol. 1987;21:253–77.


